What can I do about varicose veins?
Varicose veins are enlarged, swollen, and twisting veins, often appearing blue or dark purple.
They happen when faulty valves in the veins allow blood to flow in the wrong direction or to pool.
More than 23 percent of all adults are thought to be affected by varicose veins. Approximately 1 in 4 adults in the United States is affected by varicose veins.
Fast facts on varicose veins
- Pregnant women are more susceptible to varicose veins.
- Symptoms can include aching legs, swollen ankles, and spider veins.
- People who are overweight have an increased risk of varicose veins.
Varicose veins are large, swollen veins that often appear on the legs and feet. They happen when the valves in the veins do not work properly, so the blood does not flow effectively.
The veins rarely need treatment for health reasons, but if swelling, aching, and painful legs result, and if there is considerable discomfort, treatment is available.
There are various options, including some home remedies.
In severe cases, a varicose vein may rupture, or develop into varicose ulcers on the skin. These will require treatment.
If the patient has no symptoms or discomfort and is not bothered by the sight of the varicose veins, treatment might not be necessary. However, if there are symptoms, treatment may be required to reduce pain or discomfort, address complications, such as leg ulcers, skin discoloration, or swelling.
Some patients may also want treatment for cosmetic reasons – they want to get rid of the “ugly” varicose veins.
Surgery
If varicose veins are large, they may need to be removed surgically. This is usually done under general anesthetic. In most cases, the patient can go home the same day – if surgery is required on both legs, they may need to spend one night in hospital.
Laser treatments are often used to close off smaller veins, and also spider veins. Strong bursts of light are applied to the vein, which gradually fades and disappears.
Ligation and stripping
Two incisions are made, one near the patient’s groin at the top of the target vein, and the other is made further down the leg, either at the ankle or knee. The top of the vein is tied up and sealed. A thin, flexible wire is threaded through the bottom of the vein and then pulled out, taking the vein with it.
This procedure does not usually require a hospital stay. Ligation and stripping can sometimes result in bruising, bleeding, and pain. In extremely rare occasions, there may be deep vein thrombosis.
After surgery, most patients will need 1-3 weeks to recover before going back to work and other normal duties. During recovery time, compression stockings are worn.
Sclerotherapy
A chemical is injected into small and medium-sized varicose veins, which scars and closes them. A few weeks later, they should fade. A vein may need to be injected more than once.
Radiofrequency ablation
A small incision is made either above or below the knee, and with the help of an ultrasound scan; a narrow tube (catheter) is threaded into the vein.
The doctor inserts a probe into the catheter, which emits radiofrequency energy. The radiofrequency energy heats up the vein, causing its walls to collapse, effectively closing it and sealing it shut. This procedure is preferred for larger varicose veins. Radiofrequency ablation is usually done with a local anesthetic.
Endovenous laser treatment
A catheter is inserted into the patient’s vein. A small laser is threaded through the catheter and positioned at the top of the target vein; it delivers short energy bursts that heat up the vein, sealing it shut.
With the aid of an ultrasound scan, the doctor threads the laser all the way up the vein, gradually burning and sealing all of it. This procedure is done under local anesthetic. There may be some nerve injury, which is usually brief.
Transilluminated powered phlebectomy
An endoscopic transilluminator (special light) is threaded through an incision under the skin so that the doctor can see which veins need to be taken out. The target veins are cut and removed with a suction device through the incision.
A general or local anesthetic may be used for this procedure. There may be some bleeding and bruising after the operation.
In the majority of cases, there is no pain, but signs and symptoms of varicose veins may include:
- veins look twisted, swollen, and lumpy (bulging)
- the veins are blue or dark purple
Some patients may also experience:
- aching legs
- legs feel heavy, especially after exercise or at night
- a minor injury to the affected area may result in longer bleeding than normal
- lipodermatosclerosis – fat under the skin just above the ankle can become hard, resulting in the skin shrinking
- swollen ankles
- telangiectasia in the affected leg (spider veins)
- there may be a shiny skin discoloration near the varicose veins, usually brownish or blue in color
- venous eczema (stasis dermatitis) – skin in the affected area is red, dry, and itchy
- when suddenly standing up, some individuals experience leg cramps
- a high percentage of people with varicose veins also have restless legs syndrome
- atrophie blanche – irregular whitish patches that look like scars appear at the ankles
Complications
Any condition in which proper blood flow is undermined has a risk of complications. However, in the majority of cases, varicose veins have no complications. If complications do occur, they may include:
- Bleeding.
- Thrombophlebitis: Blood clots in the vein of the leg cause inflammation of the vein.
- Chronic venous insufficiency – the skin does not exchange oxygen, nutrients, and waste products with the blood properly because the blood flow is weak. Chronic venous insufficiency is not caused by varicose veins, but the two entities are closely related.
People with chronic venous insufficiency may develop varicose eczema, lipodermatosclerosis (hard and tight skin), and venous ulcers. Venous ulcers classically form around ankles and are often preceded by a discolored area. It is important to get medical evaluation for chronic venous insufficiency.
The veins have one-way valves so that the blood can travel in only one direction. If the walls of the vein become stretched and less flexible (elastic), the valves may get weaker. A weakened valve can allow blood to leak backward and eventually flow in the opposite direction. When this occurs, blood can accumulate in the vein(s), which then become enlarged and swollen.
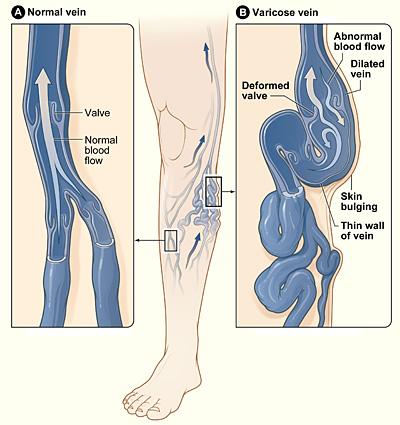
Figure A shows a normal vein with a properly working valve. In Figure B, the varicose vein has a faulty valve, the walls of the vein are thin and stretched.
Image credit: National Heart Lung and Blood Institute.
The veins furthest from the heart are most often affected, such as those in the legs. This is because gravity makes it harder for blood to flow back to the heart. Any condition that puts pressure on the abdomen has the potential to cause varicose veins; for instance, pregnancy, constipation and, in rare cases, tumors.
Risk factors
Experts are not sure why the walls of veins stretch or why the valves become faulty. In many cases, it occurs for no clear reason. However, some potential risk factors include:
- menopause
- pregnancy
- being aged over 50
- standing for long periods
- family history of varicose veins
- obesity
The following risk factors are linked to a higher risk of having varicose veins:
- Gender: Varicose veins affect women more often than males. It may be that female hormones relax veins. If so, taking birth control pills or hormone therapy (HT) might contribute.
- Genetics: Varicose veins often run in families.
- Obesity: Being overweight or obese increases the risk of varicose veins.
- Age: The risk increases with age, due to wear and tear on vein valves.
- Some jobs: An individual who has to spend a long time standing at work may have a higher chance of varicose veins.
Pregnancy and varicose veins
Women are much more likely to develop varicose veins during their pregnancy than at any other time in their lives. Pregnant women have much more blood in their body; this places extra pressure on the circulatory system.
Additionally, changes in hormone levels can lead to a relaxation of the blood vessel walls. Both these factors raise the risk of having varicose veins.
As the uterus (womb) grows, there is more pressure on the veins in the mother’s pelvic area. In the majority of cases, the varicose veins go away after the pregnancy is over; this is not always the case, and sometimes, even if the varicose veins improve, there may be some left visible.
Measures can be taken at home to improve pain and prevent varicose veins from worsening.
These include:
- exercising
- losing weight
- raising the legs
- avoiding prolonged standing or sitting
There are also many over-the-counter natural treatments, usually topical creams and emollients.
These can help soothe pain, and improve comfort and they may improve the general appearance of varicose veins.
Compression stockings
Compression stockings squeeze the patient’s legs and improve circulation.
They work are tight around the ankles and loose further up the leg. In this way, compression stockings encourage proper blood flow upwards, against gravity and back towards the heart.
Compression stockings may help with discomfort, pain, and swelling, but research has not confirmed whether they stop the varicose veins from worsening, or even prevent them. Studies have had mixed and conflicting results.
The stockings make some people’s skin dry and flaky. If this happens, it is important to tell a doctor.
To reduce the risk of developing varicose veins:
- get plenty of exercise, for example, walking
- maintain a healthy weight
- avoid standing still for too long
- do not sit with the legs crossed
- sit or sleep with your feet raised on a pillow
Anyone who has to stand for their job should try to move around at least once every 30 minutes.
A physical examination, mainly visual, by a doctor will decide whether or not a patient has varicose veins. The patient will be asked to stand while the doctor checks for signs of swelling.
The following diagnostic tests are sometimes ordered:
- Doppler test: An ultrasound scan to check the direction of blood flow in the veins. This test also checks for blood clots or obstructions in the veins.
- Color duplex ultrasound scan: This provides color images of the structure of veins, which helps the doctor identify any abnormalities. It can also measure the speed of blood flow.
The patient may also be asked questions about the symptoms. In some cases, a doctor might refer the patient to a vascular specialist.

ليست هناك تعليقات:
إرسال تعليق